5.27 Concealed/Denied Pregnancy
If a birth is suspected to have taken place, immediate steps will need to be taken to confirm the location, wellbeing and safety of the baby or foetus. In both cases this will require immediate action Call 999 for Emergency Medical Care and a Referral to CADS (Children’s Advice and Duty Service) 0300 800 8021
A concealed or denied pregnancy is where a woman has not accessed antenatal care before 20 weeks. There is no typical set of circumstances associated with concealed/denied pregnancy, though it can present as high risks to the unborn baby or infant once delivered. In some cases, a woman may be in denial of her pregnancy because of mental illness, substance misuse or as a result of a history of loss of a child or children. The purpose of this guidance is to understand the circumstances and factors that can lead to women denying, concealing, being unable to accept, or being unaware of a pregnancy, and how professionals should respond. This guidance uses the terms “woman” or “mother” throughout. These should be taken to include girls under 18 and people who do not identify as women but who are pregnant. Similarly, where the term “parents” is used, this should be taken to include anyone who has main responsibility for caring for a baby (Nice guidance on antenatal care 2021).
A concealed/denied pregnancy is when:
- a woman is unaware of or unable to accept the existence of her pregnancy
- physical changes to the body may not be present or misinterpreted
- a woman may be intellectually aware of the pregnancy but continue to think, feel, and behave as though she is not pregnant
- a woman knows she is pregnant but does not tell any health professional
- when a woman tells a professional but conceals the fact that she is not accessing antenatal care
- when a pregnant woman tells another person or persons, and they conceal/do not disclose the fact to professionals
What action to take when a concealed/denied pregnancy is suspected
If there is a suspicion of a concealed/denied pregnancy, a woman should be strongly encouraged to go directly to their midwife to access antenatal care. If a woman contacts her GP surgery, she can access support to register with midwifery services. Every effort should be made to resolve the issue of whether a woman is pregnant or not, through direct but sensitive discussion. No one can be forced to take a pregnancy test or any other medical examination. If a woman refuses a pregnancy test to confirm or rule out a pregnancy, professionals should suspect that she is pregnant, however each case is Individual and each woman has a choice, women can decline antenatal care. Professional Joint Agency Group Supervision should be considered with other agencies involved in the case.
Professionals must balance the need to maintain confidentiality with the potential risk to the unborn child and the mother’s health and wellbeing Where there is a strong suspicion of a concealed/ denied pregnancy and significant additional risk factors relating to the welfare of the unborn child and pregnant woman, it is necessary to share this irrespective of consent for information sharing(see below guidance on GDPR and Information sharing).
Professionals need to maintain their professional curiosity to explore the reasons why a woman may deny a pregnancy or choose not to attend appointments or avoid appointments by frequently cancelling them rather than attend and an understanding of trauma responses by pregnant women and how to engage them in care. Throughout the assessment process referrals and signposting can be made to unplanned pregnancy services if the woman does not want to continue with the pregnancy. All professionals should remain aware of the possibility of pregnancy in women of childbearing age, regardless of their contraceptive status.
Some pregnant women may present as concealing a pregnancy, but in reality are not seeking to avoid maternity care. They may have:-
- Lack of knowledge about the expectation to make contact with health services, particularly if there is a very different expectation in their own country or culture
- Language skills can act as a significant barrier to knowing when or how to contact maternity services
- The prohibitive cost of travel to appointments could also be a factor
- For women who have no recourse to public funds, the fact of being charged for healthcare can act as a barrier to women attending for antenatal care. What may present as a concealed pregnancy could also be seen as a reasonable decision to conserve funds while preparing for a baby
- Lack of ID with an address may also act as a barrier to women proving their entitlement to NHS care, particularly if they have no permanent address, have been trafficked, have moved frequently, or are living in temporary accommodation.
An interpreter should always be used when a woman’s communication or English is a second language and would prevent a comprehensive assessment or disclosure of abuse.
Each NHS trust in Norfolk has a process to follow when women do not attend (DNA) planned antenatal appointments (Please refer to each organisations policies and procedures). Understanding that midwifery care only begins with a confirmed pregnancy and self-referral from the woman. In concealed/denied pregnancies there may be no evidence or the woman denies the pregnancy if approached by professionals or deliberately misleading professionals that there has been a termination or miscarriage. Every opportunity should be given to engage the woman in antenatal services advice and guidance about outcomes for herself and the unborn baby if appropriate care is not sought.
Women who decline all maternity care and continue to deny a pregnancy but there is a strong suspicion of pregnancy all professionals should be part of multi-agency meetings including children’s social care, midwifery, primary care and health visiting services, where appropriate unplanned pregnancy services and police to ensure everybody is included in the risk management, concerns and plans for an estimated pregnancy/delivery guide. Multi-agency alerts should be considered including ambulance and out of hours services.
Safeguarding or Joint Agency Group supervision and/or a consultation with CADS to discuss concerns should always be considered.
If there is a suspicion of a young person under the age of 18 is pregnant and may be considered a Child In Need or Child in need of Protection in their own right a consultation with CADS should be considered. Health professionals will need to consider Gillick competency if a young person under the age of 16 wants to receive treatment without consent or knowledge of their parent or carer. All young people should be encouraged to include their parent/carer in their pregnancy by professionals and they may need professional support to have those conversations with family/carers unless it would put them at significant risk of harm. It is important for professionals to exercise curiosity at each contact with the young person. Consider the information shared with them, apply to safeguarding knowledge and to then translate to current /ongoing risk, this will inform multi agency decision making.
All teenagers will be offered an enhanced offer of care from Universal health services including midwifery, healthy child programme and/or Family Nurse Partnership (FNP offer commenced under 28 weeks gestation.)
See flowchart for guidance on what steps to take:
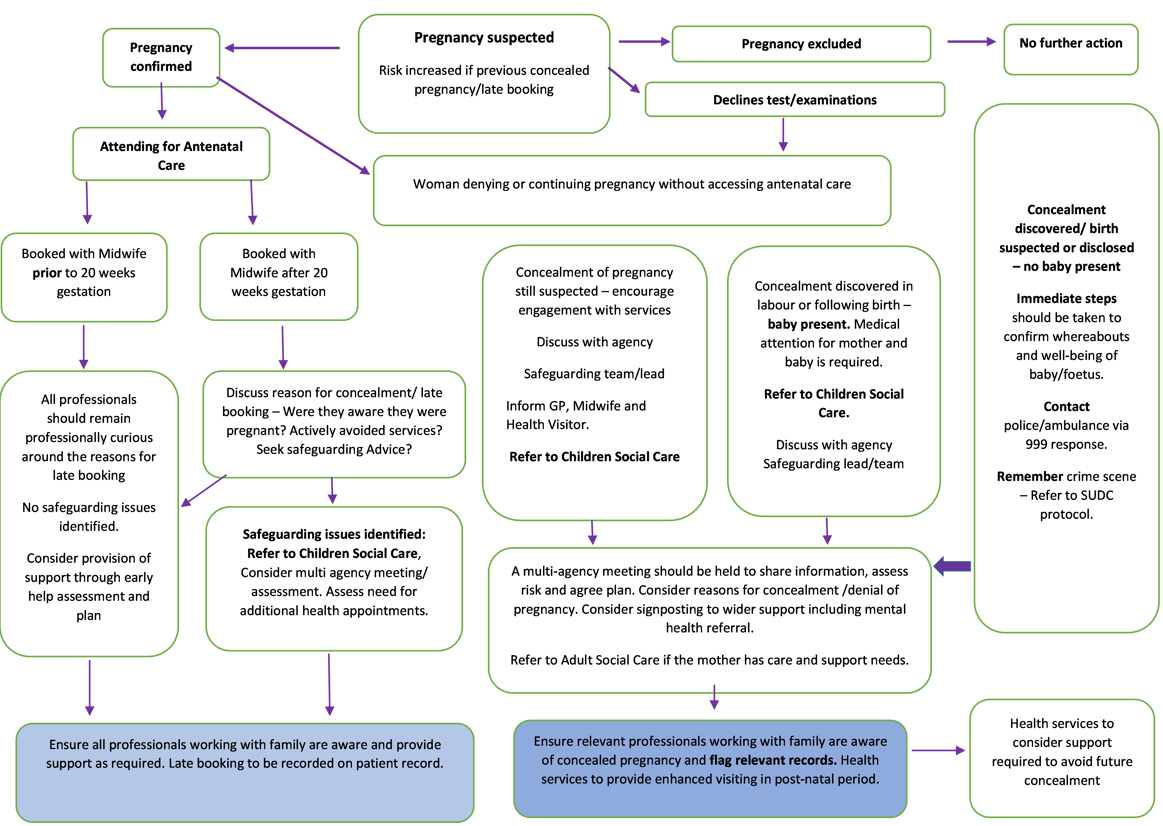
With thanks for Pan-Lancashire Safeguarding Children Partnership for adaptation of their flowchart
What action to take when a concealed/denied pregnancy is expected or confirmed
Maternity services or unplanned pregnancy services will often be the agency within whom a woman is in contact at the point a pregnancy is revealed or confirmed. However, all professionals have a responsibility for supporting a woman to access and attend antenatal care at the point a concealed pregnancy is confirmed or suspected. Any individual or agency could become aware through a woman sharing that she is pregnant or going into labour. It is vital that information about the concealment or denial is shared with relevant agencies, to ensure that there are appropriate responses, and risks can be fully assessed and managed by all professional involved in her care. Every event of concealed or denied pregnancy requires a conversation about what support may be needed, and what risks exist, as a result of a concealed or denied pregnancy, a consultation should be held with CADS
When concealment of a pregnancy in the community is revealed and a birth is suspected, immediate steps must be taken to confirm the whereabouts and wellbeing of the baby/foetus, by the professional or agency who has this information. This is likely to require a police/ambulance response via 999 and referral to CADS .
If a woman gives birth in hospital or attends hospital subsequent to a concealed/denied pregnancy, midwifery services will follow their hospital guidelines regarding concealed or undiagnosed pregnancy where they are in existence, antenatal care and ‘did not attend’ policies, alongside safeguarding policies and procedures. All professionals will be professionally curious and have conversations with a mother to highlight concerns which will inform the assessment and referral to Children’s Social Care. Consideration should be made for a trauma informed approach and understanding of the woman’s reasoning for the concealed/denied pregnancy. Prior to discharging a mother and baby, midwives will have undertaken a thorough assessment, liaison with appropriate universal health service including GP, Health Visitor, mental health professionals (where appropriate) and CADS to ensure continuity of care.
In Brief
Risks when a woman and baby does not have medical care during pregnancy
Risks to mother
- If a woman has not had her health monitored during pregnancy, underlying or emerging medical conditions will not be known or treated. Likewise, obstetric problems may go undiagnosed. Any potential risks to the mother and child may not be identified
- An unassisted delivery can be very dangerous for both mother and baby, as complications or birth injuries can occur during labour and delivery
- If a woman is denying a pregnancy, the sudden effects of going into labour and giving birth could be traumatic
- The reasons for a concealed or denied pregnancy could present particular risks to a mother and could lead to a risk of harm when the pregnancy is revealed. This might be due to fear of violence or harm, or recrimination from others, for many reasons including paternity of the baby, sexual abuse or exploitation, trafficking
- A woman will be without support and information given during pregnancy, and the opportunity to provide early intervention or support will not be possible
Risks to baby
- Concealment and denial of a pregnancy can lead to a fatal outcome, regardless of a mother’s intention. Some babies who are born with serious health issues will need to receive immediate medical care to avoid death or serious impairment of their health
- An unassisted delivery can be very dangerous for both mother and baby, as complications or birth injuries can occur during labour and delivery
- If the health and development of the baby have not been monitored during pregnancy, foetal abnormalities or underlying medical conditions will be undetected
- If the health and development of the baby have not been monitored during pregnancy, this could lead to potentially harmful medications being prescribed by a medical practitioner who is not aware of the pregnancy. Some medication can affect an unborn baby’s health and development
- If a mother drinks alcohol or uses drugs through a concealed pregnancy, support services will be unable to provide advice to reduce the use of substances which could affect the foetus’s health or development. If alcohol or substance misuse has continued during pregnancy, this increases risks to a child’s health following delivery
- When a pregnancy has been concealed or denied, this could indicate a lack of willingness or capacity to consider the baby’s health needs. Parents are likely to be unprepared for pregnancy or birth. Bonding between parents and a baby begins before birth, and without this it may be more difficult for an emotional bond and parental attachment to develop.
Legal context of concealed or denied pregnancy
- A baby does not exist as a legal entity until he/she is born. Plans can be made to protect a baby when he/she is born, but no action can be taken to safeguard them until this point.
In terms of law an unborn child does not have legal rights until birth and therefore we cannot seek orders from the court to protect an individual child until that time. Nevertheless, an unborn child can be subject to a s47 investigation and can be protected by registration on the Child protection register. An unborn can also be protected if a mother is not cooperating with a treatment plan that puts her and the baby medically at risk although that is subject to her capacity to make her own decisions even if that places either herself or unborn child in mortal danger.
- A baby is considered to be born if he/she has taken a breath. This may include situations which are later classified as Sudden Infant Death in Childhood (SUDIC). Police will be involved if there is an investigation when a child dies, or an infant is found dead at birth.
A baby is considered born when it has a separate existence from its mother. (See Below for reference)
Further Legal Frameworks to consider
- Free birth, also called unassisted birth, is when a woman has no medical support. It is not illegal and a woman intending to freebirth is not committing a crime, but if there is somebody present that performs medical actions or is monitoring the birth, this person is committing a crime and could be prosecuted.
There is no specific definition for a freebirth but in broad terms it means a woman who intentionally gives birth to her baby without a doctor or midwife present. Some prefer the term unassisted childbirth. Just like any other medical procedure there is no requirement in law for you to receive medical care or treatment unless you do not have the medical capacity to make decisions for yourself. The decision to have an unassisted birth may however be considered a risk factor when looking at a parent’s ability to protect their child as it can increase the risk to the child of significant harm or death.
- If the woman is aged under 18, then consideration will be given to whether she is a vulnerable young person. If she is less than 16 years old, then a criminal offence may have been committed and this may have to be investigated.
Mothers under the age of 18 years may also be at higher risk. According to the Nuffield Trust infant mortality rates are 60% higher for babies born to teenage mothers. This is partly associated with the higher medical risks to adolescent mothers with higher risks of eclampsia, puerperal endometritis and infection than mothers aged over 20 to 24 years according to the World Health Organisation in September 2022. There are also social vulnerabilities for this age range with greater risk of emotional, physical and sexual exploitation.
Under the Sexual Offences Act 2003, children under the age of 13 years are not considered able or competent to give consent to sexual activity and penetrative sex is classed as rape. Sexual activity under the age of 16 years is also a criminal offence although decisions to prosecute are made on the basis of the relative ages of the persons involved, and whether there was concern over coercion and competence of the young person’s decision making. Sexual activity between an adult and child under 16 years is an offence and this acknowledges the vulnerability of teenagers even if they do not view themselves in that way. Even if over the age of 16 years a child may still be at risk and child protection process can apply.
CAPACITY
- Where there is a concern about a woman’s ability to make an informed decision about proposed medical treatment, including obstetric treatment, in some circumstances legal action may be available to protect their health and the health of the unborn child. The Mental Capacity Act 2005 states that a person must be assumed to have capacity unless it is proven that she does not. A person is not to be treated as unable to make a decision because they make an unwise decision. It may be that a pregnant woman or girl denying her pregnancy is suffering from a mental illness and this is considered an impairment of mind or brain, as stated in the act, but in most cases of concealed and denied pregnancy this is unlikely to be the case.
- Adults who have the capacity to understand the consequences of their actions are able to make unwise decisions, e.g a decision not to access antenatal care.
The Mental capacity Act 2005 has guiding principles set out in s1 of the Act
(2) A person must be assumed to have capacity unless it is established that he lacks capacity.
(3) A person is not to be treated as unable to make a decision unless all practicable steps to help him to do so have been taken without success.
(4) A person is not to be treated as unable to make a decision merely because he makes an unwise decision.
(5) An act done, or decision made, under this Act for or on behalf of a person who lacks capacity must be done, or made, in his best interests.
(6) Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person’s rights and freedom of action.
This means you can make the necessary enquiries to establish capacity but you must not make assumptions or conclude they don’t have capacity if they put themselves or their baby at greater risk. - Some incidences of concealed or denied pregnancy may involve women who are particularly vulnerable, for example through trafficking or modern slavery, and legal action may be needed to safeguard the woman as well as child.
The Modern Slavery Act 2015 consolidates the existing offences of human trafficking, and slavery. It includes trafficking for all forms of exploitation. Even if someone comes voluntarily to the UK they may subsequently be exploited as a result of overstaying a Visa or when they don’t have a right to live and work in the UK. It is sometimes difficult to determine whether a person does not seek medical assistance because they fear deportation, or they are subject to coercive control.
Disclosure
Practitioners should be proactive in sharing information as early as possible to help identify, assess and respond to risks or concerns about the safety and welfare of children, whether this is when problems are first emerging, or where a child is already known to local authority children’s social care (e.g. they are being supported as a child in need or have a child protection plan). Practitioners should be alert to sharing important information about any adults with whom that child has contact, which may impact the child’s safety or welfare. (Working Together to Safeguard Children 2023)
When working with children and young people, it’s important to keep in mind:
1. Timely information sharing is key to safeguarding and promoting the welfare of children. It enables intervention that crucially tackles problems at an early stage.
2. If a child is at risk or suffering significant harm, the law supports you to share information without consent.
General Data Protection regulation (GDPR) Data Protection Act 2018, confidentiality and Article 8 of the ECHR 1998 as well as the Human Rights Act 1998, all apply to decisions which impact upon an individual’s right to a private family life, and therefore have to be carefully considered and weighed.
It is important that we are open and honest with individuals and families from when we start working with them about why, how and with whom information will or could be shared and seek agreement unless it is unsafe or inappropriate to do so.
These are important and serious rights, ones which may be breached for reasons of necessity, but only within proportionate boundaries. The right to confidentiality and the right to breach are equal rights, neither is more important than the other.
Unless there’s a statutory duty or a court order to share information the decision to share where we do not have consent under the GDPR and Data Protection Act 2018 is if in your professional judgement there is a lawful basis to do so such as safety may be at risk. The Judgment needs to be based on the facts of the case to decide whether to share and what should be shared. When you gather personal information you need to be clear with them the basis upon which you are doing it. Where you don’t have their consent be aware that that person may not expect you to share the information.
When you’re making these decisions, the safety and welfare of the child must be your key consideration. You must have a clear and legitimate purpose for sharing information however you need to also consider the safety and well-being of the person whose information you are sharing and any others who may be affected by your decision.
When facing a safeguarding risk that may require the release of information NCC must consider the following :
i) Any disclosure must justify its purpose:
ii) Such personal and confidential information should only be shared if absolutely necessary;
iii) The minimum information necessary should be shared:
iv) Sharing should only be on a need-to-know basis, not with those who do not need to know;
v) The duty to share is as important as the duty to disclose;
vi) Consider the issues objectively and impartially. Make sure your own cultural background or religious beliefs don't affect your decisions.
Personal information collected by one organisation can be disclosed to another
Unless the information is to be used for a purpose incompatible with the purpose it was originally collected for. In the case of children in need, or children at risk of significant harm, it is difficult to foresee circumstances where information law would be a barrier to sharing personal information with other practitioners.
The Information Sharing Golden Rules are
1. Necessary: the gravity of the risk, the extent of the risk and the fact that unidentified persons are at risk, and not identified individuals, makes it more difficult to protect and so the risk is greater; there is then the inability to protect others, without sharing and is it is difficult to protect against a risk which is unknown and not foreseen. You should consider the impact on the information subject and third parties. This includes information within a family and you should not make assumptions as to what may be known already.
2. Proportionate: or the same reasons as above, disclosure is proportionate but it must be limited as far as possible eg X poses a risk of sexual harm to young children, no more detail is proportionate; Information must be proportionate to the need and level of risk.
3. Relevant: the risk assessment needs to consider the specific risk posed, the level of that risk to the individual or individuals to be informed. Eg if it is a risk to young children is it necessary to share with an environment where there may be no young children. It needs to allow others to do their job effectively and make informed decisions and that may include family members in a safeguarding role or network.
4. Adequate: disclosure of a limited nature may be adequate to ensure that the alarm is raised and further information sought – how much do we need to share to trigger caution or challenge? It should be accurate and up to date, distinguish fact from opinion. Does it need to identify an individual to reduce the risk?
5. Accurate: Stay with disclosure that is on solid ground. For example what evidence is there a risk? and how solid is that evidence. We should consider what professional input into a risk assessment or the source. If it is hearsay is that sufficient to assess a risk and should we be stress testing or challenging the information; Also is it up to date? Historical information can be shared but this should be explained.
6. Timely: no good sharing the information after a risk has lessened; Information needs to be shared when it is needed to reduce the risk of missed opportunities to support and protect a child. This is especially true in an emergency situation. This may prevent seeking and obtaining consent about the information to be shared.
7. Secure: information should be shared securely. The level of security depends upon the personal nature of what is disclosed. Be aware that emails are not secure and make plans for how the information can be contained once shared. – one hard copy only and returnable or simply shared and not handed over etc …Make sure you are aware of Norfolk County Council’s policy for sharing information securely and seek advice if you are not sure what options there may be.
8. Record: make sure you record any decision you make with regard to sharing even if it not to share. If you decide to share make sure you record what you have shared, with whom and for what purpose. If it is not to share record the reasons. Do not keep the information longer than necessary – seek advice if you are unsure.
9. Consider getting consent
Ask for consent to share confidential information unless:
1. Asking for consent may increase the risk of significant harm to the child or young person
2. A delay in sharing information may increase the risk of harm to the child or young person.
The GDPR and Data Protection Act 2018 do not prevent, or limit, the sharing of information for the purposes of keeping children and young people safe.
To effectively share information:
- all practitioners should be confident of the processing conditions, which allow them to store, and share, the information that they need to carry out their safeguarding role. Information which is relevant to safeguarding will often be data which is considered ‘special category personal data’ meaning it is sensitive and personal
- where practitioners need to share special category personal data, they should be aware that the Data Protection Act 2018 includes ‘safeguarding of children and individuals at risk’ as a condition that allows practitioners to share information without consent
- information can be shared legally without consent, if a practitioner is unable to, cannot be reasonably expected to gain consent from the individual, or if to gain consent could place a child at risk
- relevant personal information can be shared lawfully if it is to keep a child or individual at risk safe from neglect or physical, emotional or mental harm, or if it is protecting their physical, mental, or emotional well-being.
REFERENCES/RESOURCES
- Department of Health (2002) Learning from Past Experience – A Review of Serious Case Reviews London: Department of Health
- Friedman, S.M. (2005) Child murder by mothers: a critical analysis of the current state of knowledge and a research agenda American Journal of Psychiatry pp.1578-87
- Information sharing Advice for practitioners providing safeguarding services to children, young people, parents and carers 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/721581/Information_sharing_advice_practitioners_safeguarding_services.pdf
- Jenkins, A., Millar, S. and Robins, J. (2011) Denial of pregnancy – a literature review and discussion of the ethical and legal issues Journal of the Royal Society of Medicine 104(7), pp.286-291
- NICE 2021 guidance on antenatal care Overview | Antenatal care | Guidance | NICE
- Pan-Lancashire Concealed and Denied Pregnancy Guidance 2020
With thanks to Pan-Lancashire Safeguarding Children Partnership for adaptation of their flowchart - (Paton v BPAS [1978] 3 WLR 687). https://www.bpas.org/media/1182/gjo_uk_patonvbritishpregnancyadvisoryservicetrustees_en.pdf
- Stenton, S. and Cohen, M (2020) Assessment of neonaticide in the setting of concealed and denied pregnancies Forensic Science, Medicine and Pathology 16(2) pp.226-233
- The Information Commissioners Office website https://ico.org.uk/
- Tighe, S. and Lalor, J. (2020) Concealed pregnancy: lessons to be learned World of Irish Nursing May 2020
- UK Visas and Immigration (2016) https://www.gov.uk/government/publications/healthcare-needs-and-pregnancy-dispersal-instruction
- Working Together to Safeguard Children (2023) https://www.gov.uk/government/publications/working-together-to-safeguard-children--2
